Diabetes is a metabolic disorder characterized by elevated blood glucose (sugar) levels, caused either by insufficient insulin production (Type 1 diabetes), by insulin resistance (Type 2), or by other factors (gestational, secondary, etc.). One of the most important tools in diagnosing, monitoring, and managing diabetes is the A1C test—also known as HbA1c, “glycated hemoglobin,” or “glycohemoglobin.” In this article, we'll explore A1C in scientific detail, including its meaning, correlation with diabetes symptoms, and the thresholds used in diagnosis and management.
What is A1C / HbA1c?
- The A1C test measures the percentage of hemoglobin molecules in red blood cells (RBCs) that have glucose attached. This process happens non-enzymatically (i.e., without specialized enzymes) and is known as glycation.
- Hemoglobin is the protein that carries oxygen in red blood cells; when glucose in the bloodstream binds to hemoglobin, those molecules become “glycated hemoglobin.” The more glucose in the blood over time, the more hemoglobin becomes glycated.
- Since red blood cells live about 2-3 months (roughly 90 days), the HbA1c gives a weighted average of blood sugar exposure over that time period. More recent glucose levels contribute more to the A1C than earlier ones.
How the A1C Test Works
- A blood sample is taken (either from a vein or sometimes capillary blood via a finger prick) and analyzed in a lab to determine the fraction of hemoglobin that is glycated.
- There is a standardized methodology: laboratories often use high-performance liquid chromatography (HPLC), immunoassays, or similar validated techniques. The results are standardized (for example, in the U.S.) against benchmark studies to ensure consistency among labs.
- Because it reflects average glucose exposure over weeks/months, the A1C is not affected by short-term fluctuations (e.g., after meals), making it more stable than a single blood glucose measurement.
What A1C Levels Mean: Normal, Prediabetes, Diabetes, and Treatment Targets
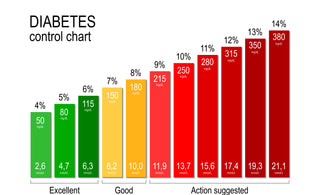
A1C results are usually interpreted using well-established thresholds, although the exact cut-off values may vary slightly depending on the country or laboratory. In general, an A1C level below 5.7 percent is considered normal and indicates healthy blood sugar regulation. People in this range are not typically classified as having diabetes, and their estimated average blood glucose usually falls under about 117 milligrams per deciliter (6.5 mmol/L).
When A1C results fall between 5.7 and 6.4 percent, the individual is placed in the category known as prediabetes. This stage reflects a higher-than-normal blood sugar level that has not yet reached the threshold for diabetes. Prediabetes signals increased risk and serves as a warning that lifestyle adjustments, such as improved nutrition, physical activity, and weight management, may help prevent progression to Type 2 diabetes.
An A1C result of 6.5 percent or higher on at least two separate tests is generally diagnostic of diabetes. At this level, blood sugar has been elevated for a sustained period, and medical evaluation is necessary to confirm the diagnosis and begin treatment.
For people already living with diabetes, healthcare professionals often set a treatment goal of keeping A1C levels below 7 percent. However, this is not a one-size-fits-all target. The ideal level may differ based on age, overall health, duration of diabetes, and the potential risks of low blood sugar episodes (hypoglycemia). Some younger and healthier individuals may aim for tighter control, while others with additional health conditions may require a more flexible goal.
Why A1C Is Used in Diabetes Diagnosis & Management
- Diagnosis: A1C is one of the accepted criteria for diagnosing Type 2 diabetes and prediabetes. It gives a long-term view of blood sugar control, which helps identify individuals whose blood sugar has been elevated for some time.
- Monitoring: For those with diabetes, A1C tests are used regularly to see how well treatments (diet, exercise, medications, insulin) are controlling average blood sugar over time. This helps reduce the risk of complications.
- Risk Assessment: Elevated A1C levels are strongly correlated with risk of long-term diabetes complications (eyes, kidneys, nerves, cardiovascular system) because chronic hyperglycemia (high blood sugar) damages blood vessels and other tissues.
Relationship Between A1C Levels and Diabetes Symptoms
High A1C does not always correlate with noticeable symptoms, especially early on. That’s because blood sugar can creep up gradually, and many people adapt to mild elevations. But when A1C is elevated enough, or if glucose fluctuates wildly, symptoms arise. Here’s how A1C levels interrelate with symptom development:
Common Diabetes Symptoms
Some of the first signs and symptoms of elevated blood sugar/diabetes include:
- Polyuria (increased urination)
- Polydipsia (increased thirst)
- Polyphagia (increased hunger)
- Fatigue, general weakness
- Blurred vision
- Slow healing of cuts or infections
- Unexplained weight loss (especially in Type 1 diabetes)
- Tingling or numbness in hands/feet (neuropathy) when glucose has been high for a while
How A1C Elevations Correspond to Symptoms
- Mild elevations (e.g., in the prediabetes range, 5.7-6.4%) may produce either subtle or no symptoms. Many individuals in this range are asymptomatic but have metabolic changes (insulin resistance, etc.).
- Once A1C reaches the diabetic threshold (≥ 6.5%) and especially if it’s significantly higher (8-10% and above), symptoms are more likely due to sustained hyperglycemia and its effect on body systems.
- The severity of symptoms (and the risk of complications) tends to increase with higher and more prolonged A1C. For example, risk for diabetic neuropathy, retinopathy, and kidney disease rises with A1C >7%, more so the higher it is, and the longer it's elevated.
Scientific Insights: Pros, Cons, and Limitations of A1C
While the A1C test is extremely useful, there are scientific and clinical limitations to be aware of.
Advantages
- Long-Term Measure: It reflects average glucose over ~2-3 months, reducing the need for frequent testing just for diagnosis.
- No Fasting Required: Unlike fasting glucose tests, A1C doesn't require you to fast. This makes it more convenient for patients.
- Predicts Complications: Strong correlations with risk of microvascular and macrovascular complications make it valuable for prognosis and guiding therapy.
Limitations & Caveats
- Variability in Red Blood Cell Lifespan: Any condition that alters RBC turnover (anemia, recent blood loss, hemoglobin variants, kidney disease, liver disease, etc.) can affect A1C results by making the measured percentage misleading.
- Differences by Ethnicity / Population: Some studies suggest that for a given average glucose, A1C may differslightly across different ethnic groups. This might result from differences in glycation rates or hemoglobin structure. Clinicians must keep this in mind.
- Not Perfect Sensitivity for Early Diabetes: An A1C-based diagnosis misses some cases that would be caught by glucose tolerance testing (OGTT) or fasting glucose. That is, some people with elevated postprandial glucose but not high enough A1C can still have diabetes risk.
How Often Should A1C Be Checked?
- For people without diabetes but with risk factors (overweight, family history, age, etc.), screening with an A1C test is recommended every 3 years, or more often if other risk factors are present.
- For people with diabetes who are meeting their goals, testing is usually done twice a year; more often (e.g., every 3 months) if therapy is changing or if blood sugar control is poor.
What Are Ideal / Target A1C Levels?
While “ideal” can vary person to person, some commonly used targets are:
- For many adults with diabetes, a target of < 7% is often considered a good target to minimize risks of complications.
- Stricter targets (e.g. ≤ 6.5%) may be appropriate for certain people (younger, fewer comorbidities, ability to manage risks of hypoglycemia).
- Looser targets may be acceptable for older adults, those with other health issues, or where an aggressive target would carry more risk (e.g., severe hypoglycemia).
How Lifestyle & Treatment Influence A1C
Since A1C reflects average glucose over several months, changes in diet, activity, weight, medications, and other factors gradually influence it.
Some interventions include:
- Dietary changes: Reducing intake of high-glycemic carbohydrates, refined sugars, increasing fiber, and spreading out carbohydrate load.
- Physical activity: Exercise improves insulin sensitivity, helps muscles uptake glucose, and lowers blood sugar levels.
- Weight management: Losing weight (if overweight or obese) can greatly reduce insulin resistance and lower A1C.
- Medication/insulin therapy: When lifestyle alone isn't sufficient, use of medications (oral hypoglycemics, insulin, etc.) is often required.
- Monitoring & adjustments: Regular monitoring (both self-monitoring of blood glucose and periodic A1C) allows adjustments to therapy.
The Link Between A1C Levels and Diabetes Complications
Chronically elevated A1C is not just about current symptoms; it is strongly associated with long-term damage.
- Microvascular complications: damage to small blood vessels — retinopathy (eyes), nephropathy (kidneys), neuropathy (nerves). Risk increases significantly with higher A1C over time.
- Macrovascular complications: cardiovascular disease (heart attack, stroke) also correlate with chronic hyperglycemia and elevated A1C.
- Also increases risk of poor wound healing, infections, vision loss, and kidney failure.
Summary: A1C, Diabetes Symptoms, and What You Should Know
- A1C is a key biomarker for blood sugar control over the past 2-3 months; it is essential for diagnosing and managing diabetes.
- Elevated A1C levels don’t always cause symptoms right away; many people have prediabetes or even early diabetes without obvious symptoms. However, as A1C rises, symptoms typically become more noticeable.
- Knowing your A1C level helps predict the risk of complications and guides treatment decisions.
- Maintaining A1C within the target range via lifestyle, diet, exercise, and medication can greatly reduce the risk of serious long-term problems.
A Word From HUGMYFEET
One of the lesser-discussed complications of diabetes is its impact on the feet. Elevated A1C levels and prolonged high blood sugar can damage blood vessels and nerves, leading to poor circulation, numbness, and slower wound healing. These issues make the feet especially vulnerable to blisters, infections, and ulcers. Wearing the right socks can play a surprisingly important role in daily foot care. At HugMyFeet, our non-binding socks are designed to reduce pressure, improve comfort, and support healthy circulation. They provide a gentle fit without restricting blood flow, making them an excellent choice for people living with diabetes who want to protect their feet while staying comfortable throughout the day.
